We treat
Jaw joint pain
Learn more about temporomandibular joint pain and its treatment
What is jaw joint pain (temporomandibular joint pain)?
Studies estimate that up to 70% of the population experience jaw joint problems, but only 5-12% seek treatment (Maini & Dua, 2023). Pain in the jaw joint can result in a wide range of problems: reduced quality of life, headaches and reduced ability to yawn and chew.
Jaw pain can manifest itself in many different ways and affect both the temporomandibular joint and the surrounding area. The pain can occur directly in the temporomandibular joint itself or in the surrounding muscles. It can also spread as referred pain, such as headaches, and manifest as more diffuse symptoms such as pain in the cheek, reduced mobility, neck pain, discomfort in the sternum due to tension in the neck muscles, tinnitus and pressure in the ears.
Jump to section [Show]

Understanding the temporomandibular joint
The anatomy of the jaw joint and its function in the body
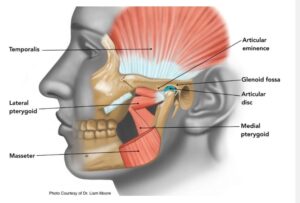
The temporomandibular joint is the connection between the mandible (lower jaw) and the temporal bone (part of the skull). This joint is surrounded by a protective joint capsule, which ensures the stability and function of the joint. As can be seen in the picture below, there is an articular disc between the two bones. This articular disc acts as a cushion, ensuring optimal movement and preventing friction between the bones.
The jaw’s movements are very unique. It can perform a hinge movement when the mouth opens and closes, but the temporomandibular joint can also slide back and forth. When the jaw is opened or closed up to 20 mm, the mandible rotates. If the mouth is opened more than 20 mm, a forward slide of the mandible occurs.
The jaw joint is primarily controlled by four muscles (seen in the picture):
- Masseter: Stabilizes the joint and elevates the mandible (closes the mouth).
- Temporalis: Elevates and moves the mandible laterally.
- Lateral pterygoid: Opens the mouth and controls the position of the articular disc during movement.
- Medial pterygoid: Helps masseter close the mouth.
All of these muscles are controlled by the trigeminal nerve, which is the 5th cranial nerve. This is particularly important because the nerve operates from the same areas in the neck and skull as the other cranial nerves. The trigeminal nerve is the largest of the cranial nerves. In addition to supplying all the muscles of the jaw, the nerve also supplies most of the face, senses pain, and is therefore often involved in headaches, both in the face and neck, as well as in sensing temperature changes, touch, the teeth, eyes, ears, and much more. The trigeminal nerve operates from the same area in the neck and brain as some of the other cranial nerves. This means that problems in the temporomandibular joint can affect other cranial nerves – and vice versa.
Common causes of jaw joint pain
The most common causes of jaw joint pain, are TMJ syndrome, arthritis, dental disease, compensation from the neck or chest, and stress:
Jaw joint pain can be divided in several ways. The most common are:
Temporomandibular dysfunction (TMD) is a broad term for a range of symptoms surrounding the jaw joint, and this disorder has several subcategories. The following criteria must be met before it can be classified as TMD:
- Crepitation: clicking, creaking, cracking, or popping sounds from the jaw joint.
- Limited jaw mobility.
- Jaw pain: pain in the jaw joint or jaw muscles (more on this later).
Temporomandibular joint syndrome (TMJS) is a subcategory of TMD. This term is used when the problem is primarily due to disorders in the jaw joint itself. Causes of this may include:
- Arthritis of the jaw joint: In osteoarthritis of the jaw joint, the disc, and in particularly advanced cases also the bones, will be broken down. Typical symptoms of osteoarthritis of the jaw are pain in the joint, which worsens with movement, and limited mobility. This falls under the category TMJS.
- Disc displacement with and without reduction: Here the disc is displaced forward, often unilaterally.
- With reduction: The disc is displaced when the mouth is closed. During a yawn, the disc’s position normalizes, which is often accompanied by pain and cracking noises.
- Without reduction: There is a permanent displacement of the disc, which no longer falls into place when yawning. The disc is stuck in the joint and blocks full movement. The pain and clicking sounds disappear, but mobility is reduced.
Muscle tension: Pain in the large chewing muscles, such as the temporalis, can result in tension headaches, typically right in front of the ear. Several factors, including stress, anxiety, and depression, have been shown to have a major impact on muscle tension around the jaw, which falls under the category of temporomandibular dysfunction.
Dental disease: A number of dental diseases can also result in jaw joint pain, such as loose teeth (periodontal disease), gum disease (gingivitis), and tooth decay (caries). The results can vary. For example, tooth pain can lead to TMJS, as you may chew primarily on one side of your mouth, which over time can change the jaw joint. Recent research has also shown that periodontal disease can affect the trigeminal nerve, which controls the muscles around the temporomandibular joint. This means that poor dental hygiene can lead to jaw pain (Bezamat et al., 2020).
Stress and other psychological factors: There is now documented evidence of a link between psychological factors and jaw pain. For example, prolonged stress can result in teeth grinding and clenching, which leads to overactivity and increased strain on the muscles and the temporomandibular joint. There is also a link between stress and altered breathing. When stressed, people tend to breathe more shallowly, and instead of using the diaphragm, neck muscles such as the sternocleidomastoid (SCM) are often used. Overactivity in this muscle can lead to a biomechanical chain reaction, where the SCM pulls the head forward, which affects the resting position of the temporomandibular joint and increases tension in the joint itself (Bartley, 2011; Salameh et al., 2015).
Diagnosing causes of jaw joint pain
Health professionals can diagnose the cause of jaw joint pain by combining examination, tests and history. The history process involves asking a series of questions to gain an overview of the nature of the pain, when it occurs and what triggers it. After the medical history, the movement of the TMJ is assessed, focusing on the range of motion and quality of movement, including any clicking sounds and pain. The surrounding muscles, especially the masticatory muscles, are then palpated to check for increased muscle tension.
Treatment of jaw joint pain
Conservative treatment of TMJ pain should always be attempted before considering surgery. This type of treatment may include relaxation exercises and strengthening exercises of the TMJ muscles, with a focus on restoring normal function to the joint. In addition, counseling on stress management and eating habits may be relevant, as these factors often have an impact on TMJ pain.
Treatment options are wide-ranging and can vary from self-care at home, which includes exercises and relieving the jaw, to medical treatment with painkillers or anti-inflammatory drugs, and in more severe cases, surgical intervention.

Self-help and home treatments
For problems in the temporomandibular joint, the following exercises can be performed several times a day. Start at a slow pace and gradually increase the range of motion. If pain occurs during the exercises, the movement or resistance is too great. Always stay within your pain threshold.
Training and relaxing the jaw muscles:
- Chin Tucks (tension release):
Performed while sitting. Straighten your shoulders and neck. Pull your head back to create a double chin. Hold this position for 3 seconds, then relax. Repeat 10 times. - Open/close mouth with resistance (strength):
- Opening against resistance: Place your thumb under your chin. Slowly open your mouth while applying slight upward pressure with your thumb to make your jaw muscles work harder to open your mouth. Repeat 10 times.
- Closing against resistance: Use your index finger or thumb to push your chin down. Open your mouth fully, then press down with your fingers to force your jaw muscles to work harder to close your mouth. Repeat 10 times.
- Lateral displacement (tension release):
Open your mouth about 2 cm and then move your jaw slowly from right to left alternately. Stay within the pain threshold and avoid forcing the movement. Repeat 10 times on each side.
Practical tips to relieve jaw joint pain at home
Some ways to relieve jaw joint pain at home include:
- Heat/cold treatment:
Using a heating pad or ice pack can provide pain relief. Heat increases blood flow and relaxes muscles, which can reduce tension, stiffness, and increase mobility. Ice can reduce inflammation in the joint. - Releasing tension of chewing muscles:
Relaxing the jaw muscles can reduce tension and thus reduce the strain on the jaw joint. - Strength training:
Strength training of the jaw muscles can have a pain-relieving effect both in the short and long term. - Mindfulness/breathing exercises:
As previously described, there is a connection between stress and jaw tension. By working on stress management and mindfulness, you can reduce pain in the jaw joint. - Dietary changes:
By eating a soft diet for a short period of time, you can reduce the strain on the jaw joint.
Osteopathy and jaw pain
The article has reviewed many factors that can affect TMJ pain, which can seem confusing. In collaboration with a therapist, a treatment plan can be developed that precisely maps out which areas need intervention.
An osteopath has thorough training in the anatomy and function of the temporomandibular joint, and can therefore help find the cause of the jaw pain. In addition, the osteopath can support you with exercises, manual treatment and advice on diet and stress management. Using manual techniques, an osteopath can, among other things, relax the trigeminal nerve or other cranial nerves, mobilize the temporomandibular joint or release tension in the jaw muscles. In osteopathy, the temporomandibular joint is seen as the last compensatory cervical vertebra, so problems in the neck, throat, chest or back can also contribute to temporomandibular joint pain.

Review of physiotherapy, dental treatments and surgery for the treatment of temporomandibular joint pain
If conservative treatments are not effective enough, the next step may be to consider surgical intervention. Typically, a laparoscopic operation will be performed first, where the temporomandibular joint is examined and treated, if possible. In some cases, an open temporomandibular joint operation may be necessary, where, for example, discs are removed or joint surfaces are smoothed.
A study has compared conservative treatment with surgical treatment and found that one year after the start of treatment there is only minimal difference between the groups in terms of pain, quality of life, function and satisfaction. However, there are advantages to starting with conservative treatment (Alam et al., 2024):
- Surgery can still be an option if conservative treatment does not work.
- You avoid anesthesia.
- Postoperative recovery is avoided with restrictions.
Medicine
In some cases, medical treatment may be considered:
- Paracetamol: Effective for temporary pain relief.
- NSAIDs (non-steroidal anti-inflammatory drugs), such as ibuprofen: Can be used for significant inflammation.
Preventing future jaw pain
There are several effective ways to prevent TMJ pain, including exercise, ergonomics, stress management, and oral hygiene:
- Jaw muscle training:
Strengthening the jaw muscles can help maintain healthy and normal function in the jaw joint. Strength training improves blood flow, which helps remove waste products and deliver nutrients to surrounding structures. At the same time, exercise can reduce muscle tension, which often contributes to pain. - Ergonomic adjustments:
Avoid sitting with your head tilted forward for long periods of time, as the position of your head can affect the stress on your jaw joint. Also try to avoid clenching your jaw by letting it hang relaxed so your teeth don’t touch each other. - Stress management:
Since stress can lead to tension in the jaw muscles, it is important to manage stress effectively. Relaxation exercises, mindfulness, and breathing exercises can help reduce muscle tension in the jaw. - Proper oral hygiene:
Good oral hygiene can prevent dental diseases such as periodontal disease, which can affect the trigeminal nerve, which controls the chewing muscles. Dental problems can also lead to chewing more on one side of the mouth, which puts unnecessary strain on the jaw joint (Temporomandibular Dysfunction (TMD).
By following this advice, you can minimize the risk of future temporomandibular joint pain and maintain healthy jaw function.

When should you seek professional help?
It is important to seek professional help for jaw joint pain in the following situations:
- Sudden decreased ability to yawn or open the mouth.
- Sudden pain in the jaw, temple, or in front of the ear.
- If the pain or discomfort does not go away on its own within a short period of time.
For persistent or worsening symptoms, it is a good idea to consult a healthcare professional for an accurate diagnosis and treatment plan.
Lifestyle changes and support
Lifestyle changes can play an important role in regulating and reducing TMJ pain. Some of the most effective measures include:
- Stress management: Reducing stress can decrease tension in the jaw muscles, which can relieve pain.
- Improving posture: Proper posture can help relieve stress on the jaw joint.
- Diet and nutrition: Eating softer foods during periods of pain can help avoid further strain on the jaw joint.
- Physical activity: Regular exercise can help improve overall body function and reduce stress.
Support from Family and Friends
Support from close relationships can also play an important role in managing temporomandibular joint pain:
- Emotional support: Having persistent pain can be frustrating, and it can help to talk to someone about your concerns in a safe environment.
- Motivation: Family and friends can encourage you to stick to lifestyle changes and exercises, which can reduce pain over time.
- Stress reduction: Close relationships can help by taking over practical tasks, which can lighten the load and reduce daily stress.
Together, lifestyle changes and support from others can create a strong foundation for managing TMJ pain more effectively.
Conclusion
Many people experience jaw joint pain and tenderness in the surrounding muscles. Jaw joint pain is often multifactorial, meaning that several different factors can play a role, such as osteoarthritis, muscle tension, oral hygiene, stress, and other psychological influences.
This often makes it difficult to manage the pain on your own. Therefore, a healthcare professional can help find the underlying cause and develop a targeted treatment plan. At the same time, support from close relationships can play an important role in maintaining lifestyle changes that can promote healthier jaw joint function.
Reference list:
Alam, M. K., Rashid, M. E., Akhter, K., Abdelghani, A., Babkair, H. A., & Sghaireen, M. G. (2024). Surgical vs. Non-Surgical Management of Temporomandibular Joint Disorders: Clinical Outcomes. Journal of Pharmacy & Bioallied Sciences (Suppl 1), S678. https://doi.org/10.4103/JPBS.JPBS_938_23
Bartley, J. (2011). Breathing and temporomandibular joint disease.Journal of Bodywork and Movement Therapies 15 (3), 291–297. https://doi.org/10.1016/J.JBMT.2010.06.002
Bezamat, M., Cunha, E. J., Modesto, A. M., Vieira, A. R., & Taboas, J. M. (2020). Aquaporin locus (12q13.12) might contribute to susceptibility of temporomandibular joint disorder associated with periodontitis.PLoS ONE, 15 (3). https://doi.org/10.1371/JOURNAL.PONE.0229245
Maini, K., & Dua, A. (2023). Temporomandibular Syndrome. National Library of Medicine, 1–10. https://www.ncbi.nlm.nih.gov/books/NBK551612/
Salameh, E., Alshaarani, F., Hamed, H. A., & Nassar, J. A. (2015). Investigation of the relationship between psychosocial stress and temporomandibular disorder in adults by measuring salivary cortisol concentration: A case-control study. Journal of Indian Prosthodontist Society, 15 (2), 148–152. https://doi.org/10.4103/0972-4052.158075
Temporomandibulær dysfunktion (TMD) – Patienthåndbogen på sundhed.dk. (n.d.). Retrieved October 12, 2024, from https://www.sundhed.dk/borger/patienthaandbogen/oere-naese-hals/sygdomme/kaeben/kaebesmerter/
Billede: https://museumdental.com/jaw-clicking-popping-explained/

Often related injuries

Jaw joint pain

Vitamin deficiency – spot & control the symptoms

Trigger finger

Brain hemorrhage

Carpal tunnel syndrome

Post-traumatic headache

Sinusitis

